Fill out the form below to receive the complete PDF guide directly in your inbox. This resource provides clear, step-by-step guidance to help you make the most of the information we’ve prepared for you.
Ethiopia
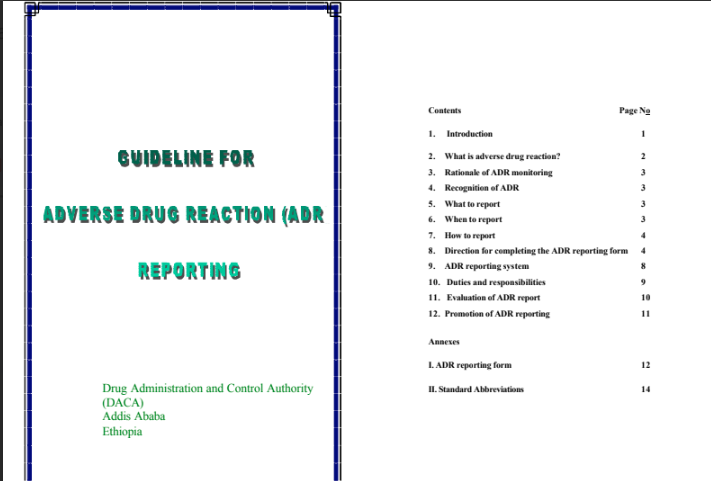
Guideline for Adverse Drug Reaction (ADR) Reporting
This guideline from Ethiopia’s Drug Administration and Control Authority (DACA) is designed to ensure consistent and complete Adverse Drug Reaction (ADR) reporting by healthcare professionals. It defines what constitutes an ADR, explains the rationale for post-marketing surveillance, and provides clear instructions on what, when, and how to report suspected reactions. The document details the structure of the national ADR reporting system, clarifies the duties of physicians, pharmacy units, and the regulatory authority, and includes the official reporting form to facilitate spontaneous reporting.
Use Cases
- Healthcare Professionals (Physicians, Dentists, etc.) – Report Suspected ADRs: To use the provided form and instructions to report any suspected ADRs they encounter, understanding that a proven causal link is not required.
- Pharmacy Units – Facilitate ADR Reporting: To ensure reporting forms are available, mail completed reports to DACA, and retain necessary documentation, acting as the institutional hub for ADR data collection.
- Drug Administration and Control Authority (DACA) – Manage the National ADR System: To collect, review, and analyze ADR reports, provide feedback, take regulatory actions like banning a drug, and communicate with international monitoring centers.
- Pharmacy and Therapeutic Committees (P&TC) – Promote Rational Drug Use: To use ADR information to revise the institutional drug list, distribute safety information to staff, and promote the rational use of medicines within their facility.
- Drug Advisory Committee – Evaluate and Recommend Action: To evaluate monitored ADR data and recommend regulatory actions to DACA, such as drug withdrawal or changes to product labeling, based on a comprehensive risk assessment.
- Reporters – Complete the ADR Form Accurately: To follow the detailed, step-by-step directions for filling out each section of the ADR reporting form, ensuring essential information on the patient, drug, and reaction is captured correctly.
Key takeaways you'll learn
The resource’s purpose is to establish a standardized, voluntary, and spontaneous ADR reporting system in Ethiopia, providing healthcare professionals with the necessary tools and knowledge to contribute to national post-marketing drug surveillance.
- Central Role of Spontaneous Reporting: The guideline establishes spontaneous reporting by health professionals as the most effective method for gathering post-marketing safety data.
- Broad Scope of Reporting: Health professionals are encouraged to report all suspected ADRs for any therapeutic agent, including minor, unexpected, and serious reactions, without needing to prove causality.
- Structured National System: A clear reporting pathway is defined: healthcare professionals report to their facility’s pharmacy unit, which then sends the report to the national authority (DACA). DACA evaluates the report, involves an expert advisory committee, and communicates with the international center in Uppsala.
- Defined Stakeholder Responsibilities: The guideline explicitly outlines the duties of each participant, from the reporting physician’s responsibility to fill the form to DACA’s mandate to analyze data and take regulatory action.
- Confidentiality and Reporter Protection: It assures reporters that all information will be kept confidential and will not be used for legal or administrative actions against the reporting professional or the patient, aiming to reduce the fear of reporting.


